Leads ECG Placement: 7 Critical Mistakes You Must Avoid Now
Understanding the correct leads ecg placement is crucial for accurate heart diagnostics. A small error can lead to misdiagnosis, delayed treatment, or unnecessary tests. Let’s dive into the essentials every healthcare provider and student must know.
What Is Leads ECG Placement and Why It Matters

Leads ecg placement refers to the precise positioning of electrodes on the body to record the heart’s electrical activity. This process forms the foundation of a 12-lead electrocardiogram (ECG), one of the most widely used diagnostic tools in cardiology. Proper placement ensures that the electrical signals from the heart are captured accurately, allowing clinicians to detect arrhythmias, ischemia, infarctions, and other cardiac abnormalities.
Anatomy Behind the ECG Signal
The heart generates electrical impulses that travel through specialized pathways, causing the myocardium to contract. These impulses can be detected on the skin surface using electrodes. The standard 12-lead ECG uses 10 electrodes—4 on the limbs and 6 on the chest—to create 12 different ‘views’ or leads of the heart’s electrical activity.
- Each lead represents a specific angle of observation of the heart.
- Leads I, II, and III are limb leads that form Einthoven’s triangle.
- Precordial (chest) leads V1–V6 provide horizontal plane views.
Misplacement of even one electrode can distort the waveform, leading to incorrect interpretations. For example, misplaced V1 and V2 can mimic right bundle branch block or anterior myocardial infarction.
“The ECG is only as good as the electrode placement.” – Dr. Philip J. Podrid, Clinical Professor of Medicine, Boston University.
Common Errors in Leads ECG Placement
Despite its routine use, incorrect leads ecg placement is surprisingly common. Studies show that up to 50% of ECGs have at least one electrode misplaced. The most frequent errors include:
- Reversal of left and right arm electrodes, altering P wave axis.
- Incorrect intercostal space for V1 and V2, leading to false anterior ST changes.
- Failure to place V4, V5, and V6 in the correct horizontal plane, causing misinterpretation of lateral wall activity.
These errors are often due to lack of training, time pressure, or patient anatomy challenges such as obesity or breast tissue.
Step-by-Step Guide to Correct Leads ECG Placement
Performing a 12-lead ECG with accurate leads ecg placement requires a systematic approach. Following a standardized protocol minimizes errors and ensures reproducibility. Below is a detailed guide endorsed by the American Heart Association (AHA) and the European Society of Cardiology (ESC).
Positioning the Limb Electrodes
The four limb electrodes (RA, LA, RL, LL) should be placed on the distal parts of the limbs, just above the wrists and ankles. The key is consistency and avoiding placement on muscle mass or bony prominences.
- RA (Right Arm): On the right forearm, near the wrist.
- LA (Left Arm): On the left forearm, near the wrist.
- RL (Right Leg): On the right lower leg, near the ankle (ground electrode).
- LL (Left Leg): On the left lower leg, near the ankle.
It’s important to note that while these electrodes are called ‘limb’ leads, they don’t need to be on the limbs themselves if the patient has amputations or dressings. In such cases, they can be placed on the torso, but symmetry must be maintained.
For more detailed guidelines, refer to the American Heart Association’s ECG standards.
Placing the Precordial (Chest) Leads
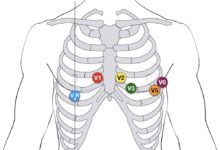
The chest leads (V1–V6) are critical for diagnosing anterior, septal, and lateral wall pathologies. Their placement must follow anatomical landmarks precisely.
- V1: 4th intercostal space, right sternal border.
- V2: 4th intercostal space, left sternal border.
- V3: Midway between V2 and V4.
- V4: 5th intercostal space, midclavicular line.
- V5: Same horizontal level as V4, anterior axillary line.
- V6: Same horizontal level as V4 and V5, midaxillary line.
One common mistake is placing V4 too high or too lateral. The 5th intercostal space is found by locating the angle of Louis (sternal angle), moving down to the 2nd rib, then counting down to the 4th space, and sliding laterally to the midclavicular line.
“A misplaced V4 can shift the entire QRS axis and mimic left anterior fascicular block.” – Journal of Electrocardiology, 2020.
Impact of Incorrect Leads ECG Placement on Diagnosis
Incorrect leads ecg placement doesn’t just produce a ‘slightly off’ tracing—it can fundamentally alter clinical interpretation. The consequences range from false positives to missed life-threatening conditions.
Misdiagnosis of Myocardial Infarction
One of the most dangerous outcomes of poor leads ecg placement is the misdiagnosis of acute myocardial infarction (MI). For example, if V1 and V2 are placed too high (e.g., in the 3rd intercostal space), it can create the appearance of ST elevation in the anterior leads, mimicking an anterior MI.
- A study in the Journal of the American College of Cardiology found that 12% of suspected anterior MIs were due to electrode misplacement.
- Conversely, if V4–V6 are placed too low, true lateral MI may be missed.
This not only leads to unnecessary interventions like thrombolysis or catheterization but also delays care for the actual underlying condition.
Altered Cardiac Axis and R-Wave Progression
The electrical axis of the heart is determined by the net direction of depolarization. Misplaced electrodes, especially in the precordial series, can shift the perceived axis.
- Reversed arm electrodes cause lead I to invert, making the QRS complex negative and mimicking dextrocardia.
- Poor R-wave progression in V1–V3 can suggest anterior infarction when it’s actually due to V3 being placed too far laterally.
These artifacts can lead to incorrect assumptions about ventricular hypertrophy, conduction blocks, or chamber enlargement.
Special Considerations in Leads ECG Placement
While standard leads ecg placement works for most patients, certain populations require modifications. These include women, obese patients, pediatric cases, and those with anatomical abnormalities.
ECG Placement in Female Patients
One of the most debated topics in leads ecg placement is how to handle breast tissue. The traditional teaching is to place V3–V6 on the breast, not underneath it. The electrodes should rest on the breast tissue itself, following the natural contour of the chest wall.
- Placing electrodes under the breast can displace them inferiorly, leading to false inferior ST depression or T-wave inversion.
- Studies show that ECGs performed with electrodes on the breast are more reproducible and accurate.
The European Society of Cardiology explicitly recommends placing electrodes on the breast to maintain anatomical accuracy.
Challenges in Obese and Pediatric Patients
Obesity can make anatomical landmarks difficult to palpate, increasing the risk of misplaced precordial leads. In such cases, ultrasound guidance or careful landmarking is recommended.
- Use the sternal angle and clavicle as fixed reference points.
- Consider using adhesive electrodes with stronger adhesion.
In pediatric patients, the heart is more horizontally oriented, and the chest wall is smaller. Leads may need to be placed closer together, but the same anatomical rules apply. V4 is still at the 5th intercostal space in the midclavicular line, even in infants.
“In pediatrics, size doesn’t change anatomy—placement must still follow landmarks.” – Pediatric Electrocardiography Guidelines, 2021.
Technological Advances and Leads ECG Placement
Modern technology is helping reduce errors in leads ecg placement. From digital ECG machines with real-time feedback to AI-powered interpretation systems, innovation is improving accuracy and training.
ECG Machines with Placement Feedback
Some newer ECG devices include built-in algorithms that detect electrode misplacement. For example, if the R-wave progression is abnormal or limb lead voltages are inconsistent, the machine may flag a possible placement error.
- GE Healthcare’s MAC 5500 HD ECG system includes a lead placement verification feature.
- Philips PageWriter TC70 offers real-time signal quality monitoring.
While not foolproof, these tools serve as a valuable second check, especially in high-volume or emergency settings.
Augmented Reality and Training Simulators
Medical schools and hospitals are adopting augmented reality (AR) and simulation models to train students in correct leads ecg placement. These systems use 3D overlays to show where electrodes should go, providing instant feedback.
- Simulaids and Laerdal offer manikins with ECG placement sensors.
- AR apps for tablets can project electrode positions onto a patient’s body using camera input.
Such tools are proving effective in reducing placement errors among novice practitioners.
Best Practices for Ensuring Accurate Leads ECG Placement
Accuracy in leads ecg placement isn’t just about following steps—it’s about cultivating a culture of precision. Here are best practices that every clinician should adopt.
Standardize the Procedure Across Teams
Hospitals and clinics should implement standardized ECG protocols. This includes:
- Using checklists for electrode placement.
- Conducting regular audits of ECG tracings for placement errors.
- Providing refresher training for staff every 6–12 months.
Standardization reduces variability and ensures that every ECG is as reliable as the last.
Double-Check Before Recording
Before starting the ECG, take 30 seconds to verify each electrode’s position. Ask a colleague to confirm if possible. This simple step can prevent costly mistakes.
- Re-palpate the 4th and 5th intercostal spaces.
- Ensure V4, V5, and V6 are on the same horizontal level.
- Confirm that limb electrodes are not on muscle or bony areas.
In emergency departments, where time is critical, this double-check can still be done efficiently with practice.
Training and Education in Leads ECG Placement
Despite its importance, leads ecg placement is often taught briefly in medical and nursing schools. Many practitioners learn on the job, leading to the propagation of errors.
Gaps in Current Medical Education
A 2019 survey published in BMC Medical Education found that only 38% of medical students could correctly place all six precordial leads. Common mistakes included placing V1 in the 2nd intercostal space or V4 in the 6th space.
- Lecture-based teaching is often insufficient without hands-on practice.
- Many curricula lack assessment of actual placement skills.
This highlights the need for more practical, competency-based training.
Effective Training Methods
To improve learning outcomes, educators should incorporate:
- Hands-on workshops with manikins and real patients.
- Video demonstrations with slow-motion landmarking.
- Peer teaching and small group sessions.
One study showed that students who practiced with immediate feedback improved accuracy by 67% compared to traditional lecture-only groups.
“You don’t learn ECG placement by reading—it’s a psychomotor skill that requires repetition.” – Dr. Teresa K. Liu-Ambrose, Neuroscientist and Educator.
What happens if ECG leads are placed incorrectly?
Incorrect leads ecg placement can lead to misdiagnosis, such as false signs of myocardial infarction, altered cardiac axis, or poor R-wave progression. This may result in unnecessary treatments or missed critical conditions.
Where should V1 and V2 be placed in leads ecg placement?
V1 is placed in the 4th intercostal space at the right sternal border, and V2 is in the 4th intercostal space at the left sternal border. These positions are critical for accurate anterior wall assessment.
Should ECG electrodes be placed on or under the breast?
Electrodes should be placed on the breast tissue, not underneath it. This ensures accurate anatomical positioning and prevents inferior displacement of leads V3–V6.
Can limb lead reversals affect ECG interpretation?
Yes, reversing the right and left arm electrodes inverts lead I and can mimic dextrocardia or alter the P wave axis. It’s one of the most common and impactful placement errors.
How can technology help improve leads ecg placement?
Modern ECG machines can detect signal inconsistencies and flag possible placement errors. Additionally, augmented reality and simulation tools provide real-time feedback during training, improving accuracy among learners.
Accurate leads ecg placement is not a minor detail—it’s a cornerstone of reliable cardiac diagnosis. From proper limb and precordial electrode positioning to understanding the impact of errors, every step matters. By following standardized protocols, leveraging technology, and investing in education, healthcare providers can ensure that every ECG tells the true story of the heart. Avoiding the common pitfalls discussed here can prevent misdiagnosis, improve patient outcomes, and uphold the integrity of cardiac care.
Further Reading: